Fish consumption, mercury exposure, and the risk of cholesterol profiles: findings from the Korea National Health and Nutrition Examination Survey 2010-2011
Article information
Abstract
In this study, the associations between mercury (Hg) exposure and cholesterol profiles were analyzed, and increased Hg levels and cholesterol profiles according to the amount of fish consumption were evaluated. Data on levels of blood Hg, the frequency of fish consumption, total blood cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and triglyceride (TG) in 3951 adults were obtained from the Korea National Health and Nutrition Examination Survey 2010-2011 database. To compare the distribution for each log-transformed indicator, Student’s t-test and analysis of variance were carried out, and the groups were classified according to the frequency of fish consumption through linear regression analysis; the association between Hg level and cholesterol profiles in each group was analyzed. The blood Hg levels (arithmetic mean, median, and geometric mean) for all target participants were 4.59, 3.66, and 3.74 µg/L, respectively. The high cholesterol group, low HDL-C group, and high TG group showed a statistically and significantly higher blood Hg level than the low-risk group. In both sexes, as the frequency of fish consumption increased, blood Hg level also increased, but TC, HDL-C, LDL-C, and TG did not show a similar trend. Increased blood Hg level showed a significant association with increased TC and LDL-C. This statistical significance was maintained in the group with less frequent fish consumption (<4 times per month), but the group with frequent fish consumption (>8 times per month) did not show a similar trend. The results of this study suggest that fish consumption increases the level of Hg exposure, and that as the level of Hg exposure increases, the levels of cholesterol profiles increase. However, this study also suggests that the levels of cholesterol profiles in those with frequent fish consumption can be diminished.
INTRODUCTION
In the general population, the major pathways of exposure to mercury (Hg) include contact with environmental contaminants, use of Hg-containing products, dental amalgam, and consumption of contaminated food including fish. Among these, fish consumption is associated with methylmercury (MeHg) exposure [1]. Whole blood total Hg level is used in the evaluation of MeHg exposure levels [2,3]. In many biomonitoring studies, a significant association between fish consumption and an increase in blood Hg level in adults and children was reported [4-9]. Moreover, it is known that the blood Hg levels of Asians, who consume a large amount of fish, are higher than those of people in Western countries [6,10].
Chronic MeHg exposure is associated with cardiovascular disease (CVD) and cholesterol profiles [11]. It has been reported that Hg increases the risk of hypertension, carotid atherosclerosis, and myocardial infarction [12-15]. It has also been reported that the Hg level in the body is significantly associated with increases in serum ferritin, systolic blood pressure, diastolic blood pressure, total cholesterol, triglyceride, and waist to hip ratio [16-18].
However, the consumption of omega-3 fatty acids due to fish consumption also has a beneficial effect in preventing CVD and coronary heart disease [19,20]. In other words, fish consumption undesirably increases MeHg and desirably increases omega-3 fatty acids at the same time in terms of CVD. Therefore, organizations such as the World Health Organization and US Food and Drug Administration have identified those who are more susceptible to the effects of Hg, and recommend consumption of an appropriate amount of fish containing higher levels of Hg rather than complete avoidance.
This study analyzed the association between Hg exposure level and cholesterols profiles as an indicator of CVD risks for dyslipidemia using biomonitoring data for the general population obtained by a national survey. The purpose of this analysis was to verify and generalize previous results regarding the association between Hg exposure and dyslipidemia risks increase in Hg level according to fish consumption and the associated the level of cholesterol profiles were evaluated.
METHODS
Population in the Korea National Health and Nutrition Examination Survey
The Korea National Health and Nutrition Examination Survey (KNNHANES) is a nationwide survey carried out by the Korea Centers for Disease Control and Prevention (KCDC). A sample representative of the entire population of Korea was determined from the results of a census; the 1st stratification was based on districts, and the 2nd stratification was based on sex and age. The KNHANES was first conducted in 1998, and the participants in the present study were the survey participants for 2010-2011; the survey questions regarding fish consumption were standardized in the KNHANES V (2010-2012). Detailed information regarding the KNHANES can be obtained from other studies [7,21].
The number of target participants in the KNHANES V (2010-2012) was 25 533, and the number in 2010-2011 was 17 476. Among these 17 476 in 2010-2011 participants, the number of adults over 19 years old was 13 165. The annual target for blood heavy metal testing in KNHANES V was approximately 2400 people over 10 years old, and the final number of target adults with valid data for both blood tests and food consumption frequency in 2010-2011 was 3951.
The KNHANES was carried out with the approval of the KCDC Committee of Ethics. The institutional review board approval numbers for the 1st (2010) and 2nd year (2011) of KNHANES V are 2010-02CON-21-C and 2011-02CON-06-C, respectively.
Data Collection
The KNHANES consists of health, nutrition, and health screening surveys. The key variables used for the analysis in this study include blood Hg level, frequency of fish consumption, and primary indicators for dyslipidemia, including TC, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and TG. In addition, other factors reported to affect the primary variables were included in the analysis. For example, smoking and alcohol consumption are associated with an increase in blood Hg level [22] as well as dyslipidemia. And obesity also [23].
The general characteristics of the target participants and the information regarding their smoking history, alcohol consumption, and family history of CVD were collected through an interview. After the interview, the height and weight were measured, and the body mass index (BMI) was calculated. The blood test items included TC, HDL-C, LDL-C, TG, and Hg concentration. Sampling was carried out in the morning, after a minimum 8-hour fast.
The 2010-2011 KNHANES used a simplified food consumption survey table consisting of 63 food items including fish. This survey asks the frequency of consumption for each food type per day, week, and month. The survey listed 9 types of fish consumed most frequently by Koreans, including mackerel, tuna, yellow fish, pollock, anchovy, fish cake, squid, clams, and pickled seafood; tuna and mackerel are known to have a high Hg content and were included in the analysis [24].
Analysis of Blood Samples
Blood TC, HDL-C, LDL-C, and TG were analyzed using enzymatic methods. A Hitachi Automatic Analyzer 7600 (Hitachi, Tokyo, Japan) was used for the analysis; the reagents used were Pureauto SCHO-N (Sekisui, Tokyo, Japan) for TC, Cholesteset N HDL (Sekisui) for HDL-C, Cholesteset LDL (Sekisui) for LDL-C, and Pureauto S TG-N (Sekisui) for TG. To evaluate the Hg level in whole blood, a 3-mL sample was collected in a commercial heparinized tube. The sample was kept in a freezer until transfer to the analysis laboratory (Neodin Medical Institute, Seoul, Korea). Hg was analyzed using the gold-amalgam method with DMA-80 (Milestone, Sorisole, Italy).
Variable Definitions
In order to evaluate the risk of dyslipidemia according to the level of Hg exposure, high-risk groups were classified into a high cholesterol group (hypercholesterolemia), a low HDL-C group (low HDL-cholesterolemia), and a high TG group (hypertriglyceridemia). The high cholesterol group included target participants whose TC level was more than 240 mg/dL after an 8-hour fast, or who were taking a cholesterol-reducing drug. The low HDL-C group included target participants whose level was below 40 mg/dL, and the high TG group include those whose level was 200 mg/dL or higher [25]. Since the high LDL-C group was not defined in the KNHANES, only the high TC group, low HDL-C group, and high TG group were assessed in this study [26].
The frequency of consumption of all types of tuna and mackerel (raw, canned, grilled, steamed, etc.) was asked, and the result was converted into the number of times consumed per month.
As confounders, BMI, smoking status, alcohol consumption and family history of CVD were considered. Family history of CVD includes parental dyslipidemia, hypertension, and hyperlipidemia.
Statistical Analysis
The Kolmogorov-Smirnov test showed that the continuous variables including blood Hg level, TC, HDL-C, LDL-C, and TG analyzed in this study had a right-skewed shape without normality. Therefore, the arithmetic mean, median, geometric mean (GM), and geometric standard deviation (GSD) were calculated in this study to report representative values. The log-transformed value was applied as a variable in statistical analysis. Student’s t-test was used to compare the distribution of blood Hg level in hypertensive and dyslipidemic high-risk groups with levels in low-risk groups, and analysis of variance was carried out to compare the distribution of each continuous variable according to the frequency of fish consumption, and to determine any increasing or decreasing tendency. The groups were classified according to the frequency of fish consumption, and linear regression analysis was carried out to analyze the correlation between the level of blood Hg exposure and dyslipidemia indicators in each group. This linear regression model included variables such as age, BMI, drinking, smoking, and family history of CVD.
Statistical significance was verified with a 95% confidence interval, and SPSS version 23 (IBM Corp., Armonk, NY, USA) was used for the analysis. The data of KNHANES apply stratified, clustered, and systematic sampling methods, not simple random sampling. In addition, to assure representation of Korean whole population, the weighting is given for the population structure of data. Therefore, the method for analyzing complex sample was applied of SPSS (IBM Corp.) [27].
RESULTS
Table 1 shows the general characteristics of the 3951 target participants in this study. The average age was 45.20 years and the sex ratio of men to women was 1.03. The median of concentrations of blood Hg was 3.7 μg/L. The proportions of target participants who consumed fish less than 4 times a month was 46.0%, followed by 25.1% for 4-8 times per month and 13.5% for more than 8 times a month. The proportion of target participants diagnosed with high cholesterol, low HDL-C, and high TG were 13.5%, 23.8%, and 12.3%, respectively.
The GM and GSD of the blood Hg level of 535 target participants included in the high cholesterol group (high-risk group) was 3.94, 1.88 μg/L, which was statistically and significantly higher than that (3.69, 1.84 μg/L) of the low-risk group (n = 3278) (p-value = 0.025). The blood Hg levels of the low HDL-C group (n = 941) were 3.95, 1.91 μg/L, respectively, and were significantly higher than those (3.67, 1.83 μg/L) of the low-risk group (n = 2924) (p-value = 0.002). The blood Hg levels of the highTG group (n = 487) were 4.37, 1.93 μg/L, respectively, and were significantly higher than those (3.60, 1.83 μg/L) of the low-risk group (n = 2615) (p-value < 0.001) (Table 2).

Comparisons of blood mercury levels in the high-risk group and low-risk group according to cholesterol profiles
Fish consumption was grouped by frequency of less than 4 times a month, 4-8 times a month, and more than 8 times a month, and the blood Hg levels and dyslipidemia indicators were compared between groups (Figure 1). In females, the blood Hg levels (GM, GSD) of the group with consumption less than 4 times a month were 3.05, and 1.75 μg/L, respectively; the levels of the group with consumption 4-8 times a month were 3.10, and 1.62 μg/L, respectively; and the levels of the group with consumption more than 8 times a month were 3.32, and 1.75 μg/L, respectively. As the frequency of fish consumption increased in females, the blood Hg level also in creased, and this trend was statistically significant (p-trend = 0.022). This trend was also statistically significant in males (p-trend < 0.001).

Frequency of blue-colored fish intake per month and the levels of blood mercury (A) and cholesterol profiles (B: total choleterol, C: HDL choleterol, D: LDL choleterol, and E: triglyceride). The p-trend calculated by analysis of variance (calculated by using log-transformed blood Hg levels). The xaxis shows the frequency of fish intake per month; blue-colored fish include tuna and mackerel. Hg, mercury; HDL, high-density lipoprotein; LDL, lowdensity lipoprotein.
The median of TC levels in the group with consumption less than 4 times a month were 188.00 mg/dL for females, and 185.00 mg/dL for males. The median of blood Hg in the group with consumption 4-8 times a month were 179.00 mg/dL for females, and 185.00 mg/dL for males; and the median in the group with consumption more than 8 times a month were 183.50 mg/dL for females, and 187.00 mg/dL for males, with no trend of significant increase or decrease (p-trend = 0.105 for females; 0.970 for males). The median of HDL-C levels in the female group with consumption less than 4 times a month was 50.00 mg/dL; the median in the female group with consumption 4-8 times a month was 50.00 mg/dL; and the median in the female group with consumption more than 8 times a month was 53.00 mg/dL, showing a trend of increase, but the male groups showed no trend of significant increase. The median of corresponding HDL-C levels in the male group with consumption less than 4 times a month was 44.00 mg/dL; the median in the male group with consumption 4-8 times a month was 45.00 mg/dL; and the median in the male group with consumption more than 8 times a month was 44.50 mg/dL (p-trend < 0.001 for females; 0.488 for males). The median of LDL-C levels in the female group with consumption less than 4 times a month was 114.00 mg/dL; the median in the female group with consumption 4-8 times a month was 107.00 mg/dL; and the median in the female group with consumption more than 8 times a month was 107.00 mg/dL (p-trend = 0.018); the median in the male group with consumption less than 4 times a month was 111.00 mg/dL; the median in the male group with consumption 4-8 times a month was 112.00 mg/dL; and the median in the male group with consumption more than 8 times a month was 114.00 mg/dL (p-trend = 0.439). The median of TG levels in the female group with consumption less than 4 times a month was 96.50 mg/dL; the median in the female group with consumption 4-8 times a month was 83.00 mg/dL; and the median in the female group with consumption more than 8 times a month was 83.00 mg/dL, showing a trend of significant decrease (p-trend < 0.001); the median in the male group with consumption less than 4 times a month was 130.00 mg/dL; the median in the male group with consumption 4-8 times a month was 125.00 mg/dL; and the median in the male group with consumption more than 8 times a month was 119.50 mg/dL, showing a trend of decrease; however, this was not statistically significant (p-trend = 0.099).
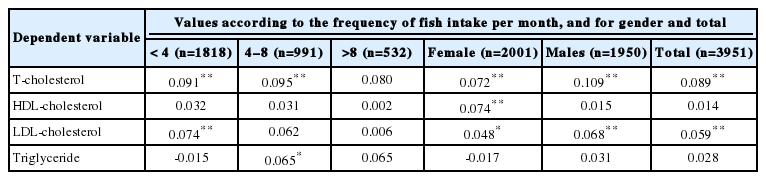
In linear regression analysis with log-transformed blood Hg level as the independent variable, and each log-transformed dyslipidemia indicator as the dependent variable, after adjustment for age, BMI, CVD family history, smoking, and alcohol consumption, increased Hg levels showed a significant association with increased TC and LDL-C. This significant association was maintained in the group with fish consumption less than 4 times a month, but disappeared in the group with consumption more than 8 times a month. In addition, increased blood Hg levels in the group with consumption more than 8 times a month did not show a significant association with either an in crease or decrease in TC, HDL-C, LDL-C, and TG. HDL-C showed a significant association with increased blood Hg level in female groups, but not in male groups or target participants (Table 3).
DISCUSSION
This study found that the level of blood Hg was high in dyslipidemic risk groups. As the frequency of fish consumption increased, blood Hg level also increased, but this trend was not observed for the dyslipidemic indicators. Among the dyslipidemic indicators, TC and LDL-C showed a trend of significant increase as the Hg level increased, but this trend was not observed in the groups with frequent fish consumption.
The hypothesis that heavy metals are risk factors for CVD and dyslipidemia has been verified by many studies. Hg and other environmental toxins are preventable exposure factors that account for demographic variations in CVD prevalence rates [28,29]. Chronic heavy metal exposure promotes red blood cell and hemoglobin synthesis [17], and lead and cadmium are heavy metals that associated with smoking, which is an important risk factor for CVD mortality [30]. Moreover, the phenomenon of blood Hg level increasing as the frequency of fish consumption increases has already been reported by many studies. In the national biomonitoring surveys performed in Canada, the Czech Republic, Germany, and the US, it was also reported that fish consumption had a significant association with increased blood Hg level [8-10,31-33]; the same result was reported for a previous KNHANES studies in Korea [5-7,34].
Thus, this study verified previous information. In addition, new information was provided, showing a high association between Hg exposure and dyslipidemic indicators in groups with less frequent fish consumption but not in groups with frequent fish consumption. Increases in the level of Hg exposure in groups with less frequent fish consumption may be caused by other factors, such as environmental or occupational exposure, dental amalgam, or smoking. Therefore, Hg exposure due to factors other than fish consumption may cause increases in cholesterol, but such effects are diminished in groups with a high frequency of fish consumption. This is shown by the findings in this study that blood Hg level increased in groups with frequent fish consumption, but that no such trend was shown for TC, HDL-C, LDL-C, and TG. Several studies suggested that a high levels of Hg exposure may diminish the cardioprotective effect of fish consumption [11,12]. These results also suggest the fish consumption may diminish the risk of dyslipidemia due to Hg exposure. Of course, there are few evidence in this study to confirm this hypothesis.
There are several limitations. First, this study has a cross-sectional design and was based on national data. In other words, since various routes and characteristics of Hg exposure were not investigated over a long period of time, the contribution of fish consumption or other factors on blood Hg level cannot be determined. Therefore, a trend was observed in the result of this study, but the result of the study cannot explain causation.
Another limitation is that specific information on the types of fish and cooking methods was not provided by the fish consumption frequency survey. Since Hg and omega-3 fatty acids content may vary according to the type of fish as well as the form of consumption, more detailed examination is necessary [35,36]. The omission of information regarding occupational exposure and dental amalgam is another limitation. These limitations result from the fact that the KNHANES is not designed for evaluation of Hg exposure alone. As well as fish consumption considered in this study, there are many other dietary characteristics can affect cholesterol profiles such as meat, sodium consumption. However, this study could not consider all these various diet or lifestyle factors.
A difference between males and females was observed for a significant portion of the results in this study. There were differences in the absolute values of each indicator as well as the trend. For example, as the frequency of fish consumption increased in females, HDL-C increased significantly, but LDL-C and TG decreased. This is of positive benefit for CVD and dyslipidemia. However, this trend was not confirmed for males. There may be some factor that accounts for differences between males and females such as smoking, drinking described in Table 1 and occupational exposure also, but the data in this study are not sufficient to identify such a factor.
HDL-C tended to increase as blood Hg level in female groups increased. HDL-C is also known to have a negative correlation with CVD [37]. Therefore, it is not clear why a positive association between the level of Hg and HDL-C was only observed in the female groups in this study. However, a trend was seen in females: as the frequency of fish consumption increased, HDL-C increased and LDL-C decreased, indicating that fish consumption had a prominent effect. This also supports a previous report that fish consumption increases HDL-C [38]. Frequent fish consumption should be associated with a low-risk of CVD because of less frequent meat consumption, but it is not certain that meat contributes more to CVD than fish [39].
In conclusion, the results of this study suggest that fish consumption increases the level of Hg exposure, and that as the level of Hg exposure increases, the risk of dyslipidemia increases. However, this study also indicates that the risk of dyslipidemia in those consuming frequent fish frequently can be diminished.
Acknowledgements
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-2013R1A1A2060215).
Notes
The author has no conflicts of interest associated with the material presented in this paper.