Humidifier disinfectant disaster: what is known and what needs to be clarified
Article information
Abstract
Objectives
After the initial investigations by the Korea Centers for Disease Control in 2011, over 1000 suspicious cases of humidifier disinfectant (HD) victims were subsequently reported by 2015, and numbers are still increasing dramatically in 2016 in the midst of the prosecutors’ office investigation. This study attempts to summarize the current understandings of the related health effects of HD based upon a systemic review of published epidemiologic studies and toxicology investigations.
Methods
Published studies of HDs were searched through PubMed and TOXLINE under the search words ‘humidifier disinfectant,’ and related reports were identified from the references and published report list of regulatory agencies including the Korean National Institute of Environmental Research, US Environmental Protection Agency, and EU European Chemicals Agency.
Results
Case reports and epidemiologic studies have reported the clinical features of severe forms of HD lung damage, together with epidemiologic findings of seasonal occurrence and demographic variations, including the heightened susceptibility of young children. Toxicological studies have reported inhalation toxicities together with positive findings of in vitro genotoxicity studies.
Conclusions
This study examined unsolved issues based on cases of upper respiratory diseases and diseases of other organs, including cancers, among suspected victims of HDs. These issues should be clarified in future research for the management and prevention of health effects from HDs and chemicals of other related household products.
Introduction
The humidifier disinfectant (HD) disaster began in April 2011 when the Korea Centers for Disease Control and Prevention (KCDC) received reports on six perinatal patients hospitalized in intensive care units. Since then, efforts have been made to find the truth regarding the health damage caused by toxic HDs and recovery efforts are still underway. Even before the prosecutor’s criminal investigation began in 2016, the details regarding the causal relationships between health damage and the exposure to HDs have been among Korea’s hotly debated issues. As social interest increased due to the criminal investigation, the issues concerning the range of health damage resulting from exposure have newly emerged. Above all, the number of people has increased to thousands at the start of the investigation and continues to rise.
Therefore, the purpose of this paper is to highlight issues which should be further clarified regarding health damage caused by toxic HDs from the perspectives of epidemiology and toxicology, in addition to summarizing the hitherto known facts. By reviewing the literature, this paper specifically tries to clarify the causal relationships (between health damage and HD) and to suggest the management systems that are needed in more detail.
Materials and Methods
PubMed and TOXLINE databases were used for the literature review on health damage caused by toxic HDs. For PubMed, ‘humidifier disinfectant’ was the key search phrase and for TOXLINE, ‘polyhexamethylene guanidine phosphate (PHMG),’ ‘oligo(2-(2-ethoxy) ethoxyethyl guanidinium (PGH),’ ‘polyhexamethylene biguanide hydrochloride (PHMB),’ ‘chloromethylisoehiasolinone (CMIT),’ ‘methylisothiazolinone (MIT),’ and other chemical names were used as the key search words.
Considering the fact that there are a lot of unpublished reports on toxicity, the reference lists of these unpublished reports and the reports from institutions studying toxic experimentation were used as sources on/for toxicity.
PubMed was used to search epidemiological and clinical reports published before June 2016. After excluding unrelated or overlapping papers, 10 articles out of 41 publications remained. In the case of content concerning the magnitude and the status of exposure to toxic HDs, two articles and two unpublished reports were found in the reference lists of other research papers. For toxicity studies, in addition to ‘PubMed’ and ‘TOXLINE’, the latest reports and published lists from the Korean National Institution of Environmental Research, US Environmental Protection Agency, and European Chemicals Agency were reviewed.
In this paper, the excerpts of the main results of these articles and reports were summarized. In cases of epidemiological investigations, the study results were organized according to research design; in cases of toxicology tests, similar chemicals were grouped together according to the toxicological assessment for easy comparison.
Results
Association Between the Usage of Humidifier Disinfectants and Pulmonary Diseases
Epidemiological Studies
The results of a case-control study of adult patients, which was conducted by the lead of KCDC in 2011, was finally published in a journal in 2014. The study of pediatric patients started after the study on adult patients, but was published in a journal in 2013 (Table 1).
Thus far, epidemiological studies that examine the causal association between HDs and health effects can be classified into two types: (1) case-control studies that examine the association between HD exposure and severe lung injuries; (2) retrospective cohort studies that examine all the family members of the victims to find out whether or not they were exposed to HDs and whether there were any subsequent incidences of diseases developing.
Each type of study shows a strong association between the use of HD and severe lung injuries even when indoor fungus or other chemical usage were taken into consideration.
The case-control studies were different in their subjects and controls: (1) children with hospital control, (2) adults with hospital control, (3) and adults with community control. However, the exposure rates to HDs in controls were 23, 26, and 22% in each study, respectively. Accordingly, the results show that exposure rate to HD in the general population was over 20% (Table 1).
The assessment committee classified severe lung injuries into four levels in the association with HD exposure: level 1 (definite), level 2 (probable), level 3 (possible), and level 4 (unlikely). In 2013, 151 victims were categorized into level 1 and level 2 upon first round assessment. At that time, daily amount of HD and time used were associated with severe lung injuries (Table 2).

Retrospective cohort study on the association between HD use and lung injury using the first round of victim registration records, as of May 2016
In addition, the number of cases (symptom development) increased as the time of exposure increased. When looking at the data in a monthly pattern, the symptoms of confirmed cases increased with the increase of months of exposure, peaked after four to six months, and then decreased, but they increased again after 12 months, showing a peak over the next four months (Figure 1). In other words, since the use of humidifiers was seasonal, the symptom breakout of confirmed cases showed a similar seasonal pattern as well.
As was revealed by case reports, the clinical conditions of toxic HDs are more affected by the environment of families than by genetic causes, because about 20% of cases reported victims within a family and less than 10% of cases had underlying lung disease (Table 3).
Radiological findings in the early period of hospitalization provided important information for patients’ prognosis with lung injuries by HDs, and clinical laboratory tests on inflammation have also been helpful to predict prognosis.
Animal Studies
Several animal studies to examine the toxicity of HDs have been reported, where the HDs were divided into two classes: (1) guanine polymer substances such as PHMG, PGH; (2) PHMB, and isothiazolinone substances such as CMIT and MIT (Table 4).
Both guanine and isothiazolinone substances showed comparable toxicities in similar concentration at acute oral and inhalation toxicity.
Chronic toxicity was found in the liver where substances absorbed through the gastrointestinal tract pass first under repeated oral exposure and in high dosage, resulting in neurotoxicity and immune-toxicity by affecting the thymus. The report that lung damage was also found in spite of oral exposure suggests the possibility that the damage could have occurred by mechanisms other than air exposure.
Under repeated inhalation exposure as in chronic toxicity tests, damage in the larynx and nasal cavities was observed in high levels for both guanine polymers and isothiazolinone substances. With guanine specifically, respiratory lesions lasted for a substantial period of time after exposure stops and in the recovery stage; therefore, the damage in respiratory organs by inhalation exposure, thereby, could be similar to humans.
The result for genotoxicity was positive before the metabolism of guanine polymer substances, while it was negative after metabolism. Therefore, in cases where absorption exposure occurs without passing through the liver such as in respiratory inhalation, the mechanism of the toxic effect should be examined. For PHMB in particular, genotoxicity and carcinogenicity of directly exposed organs through direct inhalation or oral exposure should be investigated since angiosarcoma develops in the liver by oral exposure.
Even though the results differ slightly, skin irritation and hypersensitivity was reported, specifically irritation and hypersensitivity to the mucous membranes, so research on the mechanism should be examined.
Further Investigation Needed Regarding Causal Relationships Between Humidifier Disinfectants and Lung Injury
Although studies have revealed the toxicity of HDs and how they cause severe lung injury, more detailed studies are needed. In particular, the following aspects related to lung injury caused by HDs are receiving attention.
Exposure conditions and characteristics of the susceptible population
Current research reports that the exposure characteristics to HDs is one of the factors that cause lung injury. Age, along with exposure conditions, also significantly increase the risk of lung injury (Figure 2). Reports show a higher prevalence of lung injury in children; therefore, there is a need for a systematic investigation of factors that cause varying levels of susceptibility by age as well as pathological information on lung injury. In this respect, further research is needed to examine how reversible the lung injury is based on the degree of exposure for a certain period of time and the intensity of continued and concentrated exposure. Furthermore, future studies are needed to examine the susceptibility factors that determine the threshold for irreversibility.
Mechanism of injury in patients with non-conventional exposure
Studies found lung injury in animals that experienced concentrated exposure to HDs through oral administration. This result raises questions about chemicals causing respiratory damage, possibly through pathways other than the respiratory organs, such as the blood stream. As such, more research is needed on the pathogenesis of fetal injuries since chemical exposure is placental. Moreover, toxicity in the reproductive system caused by inhaled chemical exposure warrants thorough investigation.
Natural course and prognostic factors of severe lung injury
More research is also needed on the recovery time and/or the prognosis of lung disease as well as factors that affect prognosis. In this regard, along with the issues addressed earlier, the impact underlying diseases may have on the causes and progression of lung disease must be examined.
Social and mental problems of the victims
In addition to investigating lung disease, social and mental issues that current victims are facing need to be addressed, specifically how to manage and treat the victims’ physical health conditions that impact their mental and social conditions.
Identification of the Magnitude and Characteristics of Humidifier Disinfectant- related Diseases
Conditions of Usage and Exposure to Humidifier Disinfectants
There are no studies that estimate the magnitude of all diseases caused by HDs. Existing research only estimates the usage of HDs and presumes the number of victims through their self-reports on symptoms.
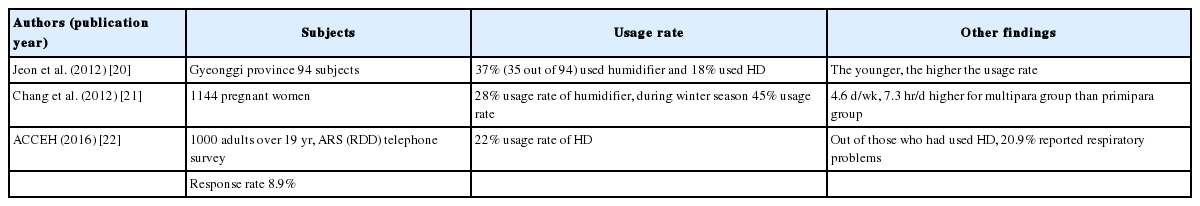
Some data sets suggest that 18 to 22% of the general population has used and been exposed to HDs. This rate is almost equal to the control group’s usage and exposure rate in the aforementioned case-control studies (Table 5).
Some studies have estimated the concentration of indoor exposure to HDs; when using the estimated exposure concentration to calculate the risk quotients for the active components in the disinfectants, the studies reported the concentration to be highly dangerous (Table 6). Furthermore, types and usage patterns of HDs were reported based on the registered cases having health effects due to HD exposure.
Scope and Magnitude of Humidifier Disinfectant-related Diseases
Range of related diseases derived from epidemiological studies
Upon reviewing the diagnosed diseases of the victims who reported health concerns in the first round of the HD injury survey, the victims were found to have diseases other than those that are lung-related (including acute interstitial pneumonitis) such as cancer, ear, nose and throat diseases, and skin conditions. This suggests that HD-related diseases could be more extensive (Table 7).

Underlying diseases and original diagnosis of suspected victims in the first round of humidifier disinfectant injury survey
In particular, of the reported victims, those in level 3 (‘possible’) and level 4 (‘unlikely’) showed diseases directly related to respiratory exposure such as chronic bronchitis, sinusitis, and rhinitis. Other reported diseases such as tuberculosis and immunity-related cancer could be also associated with respiratory exposure.
Range of related diseases derived from animal studies
Currently, animal studies report that HDs affect not only lung tissue but also various other organs.
First of all, acute toxicity effects from oral exposure are reported to cause the following: direct damage on the gastrointestinal mucosa, hepatotoxicity accompanied by prolonged prothrombin coagulation time and changes in cholesterol level, neurotoxicity with seizures, and immunotoxicity along with changes in the thymus and immunocytes. Damage to lung tissue from oral exposure has also been reported. These reports collectively suggest the possibility of oral absorption affecting lung tissue. However, in order to understand the scope of HD-related diseases that significantly affect humans, research is needed to examine what kinds of secondary damage occurs after primary damage is done to the main target organs when exposed to concentrated toxins. Furthermore, studies must also identify what initial damage occurs in cases of low concentration exposure.
Furthermore, acute toxicity through inhalation has been reported to cause damage to the upper respiratory and whole respiratory tract including the lungs, bronchus, larynx, and nasal cavity. The direct damage caused by concentrated inhalation needs to be distinguished from those which are recoverable and those which are irreversible.
On the other hand, both guanine polymers and isothiazolinone have been reported to cause skin and mucous irritation and allergic sensitization when exposed in low concentration for an extended period of time. Isothiazolinone, specifically, is widely found and all organs exposed to it are presumably directly affected based on certain levels of cell toxicity. Furthermore, some suggest that the substances may become absorbed in the systemic circulation when exposed chronically which could cause genetic toxicity, reproductive toxicity, and cancer. Therefore, further studies should investigate the health effects and damage HDs may have on all organs of the body based on the toxicants’ rate of exposure, absorption, metabolism, damage, and recovery in different exposure conditions such as exposure concentration, frequency, and duration.
In conclusion, reports on toxicity suggest a wider range of affected organs throughout the body that goes beyond severe lung disease.
Estimation of the magnitude of all diseases related with humidifier disinfectant exposure
According to the previous studies, approximately 11 million people, or 22% of the general population (Table 5), have been exposed to substances in HDs. With reference to the survey results submitted to court regarding the degree of exposure, two out of 60 were exposed to highly concentrated amounts of toxicants. This means approximately three million people were exposed to levels higher than the ‘no observed adverse effect’ level on a toxicological screening. This figure may be used to estimate the magnitude of all diseases related with HD exposure.
Future Research on Humidifier Disinfectant-related Diseases Other Than Lung Injury
In order to identify the magnitude and range of all health effects caused by HDs exposure, research on the following issues are crucial.
Current animal experiments are conducted based on standardized methods, following a consistent schedule, frequency, and period of exposure. Unlike the controlled environment used in animal testing, humans can be exposed 24 hours a day, seven days a week, all year. Future animal study, therefore, needs to make adjustments to examine the effects of concentrated and continuous exposure without a period of recovery. Studies are needed to investigate in acute exposure how the effects will vary in accordance to the changes in the concentration level of exposure, duration, and frequency of exposure along with age difference. Furthermore, studies should examine various target organs in varying stages of exposure in order to measure the range of health effects caused by HD exposure. For more accurate measurements, future investigations should first research toxicokinetics for the main exposure pathways and discover how toxicants are absorbed and metabolized via each route (Table 8).

Variables of manipulation in animal toxicology study on major chemicals used for humidifier disinfectants
Meanwhile, the range of health effects that have been reported by HD victims is partly centered around mass media coverage data, which could create discrepancies in actual users. A more systematic investigation is needed, considering the general population as study subjects and the conditions of actual usage, exposure, and side effect occurrences to pursue whether the study subjects received medical treatment and reported their conditions. With this new data set on health effects, researchers can cross-check data from previous studies and try to estimate the magnitude of each health effect by comparison of the types and degrees of health effects between data and by using the capturerecapture method.
In addition, follow-up studies on factors that affect susceptibility can provide insight into understanding all diseases’ natural courses, especially for diseases that have long latent periods, such as cancer, or diseases that may cause secondary health damage.
Lastly, comprehensive socio-psychological studies, such as family relations, social activity, damage compensation, types of support and its relevance, and mental and behavioral effects and their changes in relation with HDs exposure are needed to understand the size and scope of health effects caused by HDs. Since most victims have been unexpectedly injured at a very young age, the whole scope of the health effects including psychological trauma and its changes over time must be evaluated.
Discussion
South Korea (hereafter Korea) is not yet fully equipped with the infrastructure—such as an overseeing agency or related legal regulations—for identifying and mediating issues regarding the injuries caused by HDs. As the current issues are being resolved, the HD case in Korea could change or new and specific plans may emerge to settle and manage the issues. In this current state, the following two points that reflect on past environmental pollution issues or track other countries’ history of environmental pollution control can help Korea to investigate the current issue and provide future guidelines.
The first point to consider is that the causal relation between severe lung injury and exposure to HDs is specific. The ‘specificity,’ a specific disease related with a specific cause, is very rare in common cause and effect relationships. Mostly, a causal relationship shows non-specific relation, i.e., various causes of a disease or various diseases for a cause. In the case of HDs and their health effects, a combination of various causes may make up a spectrum of effects from specific to non-specific. The specific causal relationship is an exceptional phenomenon such as mesothelioma caused by exposure to asbestos. For example, lung cancer is considered the more significant effect of exposure to asbestos than mesothelioma, in which the causal relationship is confirmed, but when the effect of smoking is taken into consideration, lung cancer is a non-specific effect of asbestos exposure. When examining toxicants and their effects on lung and respiratory lesions, the most common complication from isethionate exposure or coal dust exposure is bronchitis, not alveolar lesions—exposure to isethionate is known to cause pulmonary fibrosis and exposure to coal dust, pneumoconiosis. As can be seen, a toxicant’s physical characteristics can determine which area will be affected, the alveoli or respiratory tract, but in practice the effects of the exposure route and of all organs that participate in the metabolic process need to be considered within the scope of health effects due to the toxicants.
The second point to consider is the need to learn from other countries’ experience. Japan’s Minamata disease, for instance, was first discovered in the 1950s, and the range of injured victims is still under debate. This example delineates the importance of a timely evaluation of damage while also being aware of the possibility that the understanding of causal relationships could change over time. In other words, institutional, administrative, and social infrastructure could be established that could prevent, detect, and manage similar future damage if we can identify and manage Korea’s HD damage and learn how to build a solution strategy in its early stages.
Korea needs improvement in the following systems: system for toxicity testing; system for cluster monitoring and epidemiologic studies; system for disease diagnosis and categorization; system for treatment; system for policy review.
In particular, the Ministry of Environment lacks an administrative structure that focuses on the health effects that hazardous substances cause, nor do they have a network that interactively engages in prevention, compensation, and policy-making across regions. All interested parties need to come together to understand the causes and effects from various angles with the a more general long-term perspective.
Notes
The authors have no conflicts of interest associated with the material presented in this paper.