Health Risks Assessment in Children for Phthalate Exposure Associated with Childcare Facilities and Indoor Playgrounds
Article information
Abstract
Objectives
This study assessed the health risks for children exposed to phthalate through several pathways including house dust, surface wipes and hand wipes in child facilities and indoor playgrounds.
Methods
The indoor samples were collected from various children's facilities (40 playrooms, 42 daycare centers, 44 kindergartens, and 42 indoor-playgrounds) in both summer (Jul-Sep, 2007) and winter (Jan-Feb, 2008). Hazard index (HI) was estimated for the non-carcinogens and the examined phthalates were diethylhexyl phthalate (DEHP), diethyl phthalate (DEP), dibutyl-n-butyl phthalate (DnBP), and butylbenzyl phthalate (BBzP). The present study examined these four kinds of samples, i.e., indoor dust, surface wipes of product and hand wipes.
Results
Among the phthalates, the detection rates of DEHP were 98% in dust samples, 100% in surface wipe samples, and 95% in hand wipe samples. In this study, phthalate levels obtained from floor dust, product surface and children's hand wipe samples were similar to or slightly less compared to previous studies. The 50th and 95th percentile value of child-sensitive materials did not exceed 1 (HI) for all subjects in all facilities.
Conclusions
For DEHP, DnBP and BBzP their detection rates through multi-routes were high and their risk based on health risk assessment was also observed to be acceptable. This study suggested that ingestion and dermal exposure could be the most important pathway of phthalates besides digestion through food.
INTRODUCTION
Among phthalates, typical endocrine disruptors, diethylhexyl phthalate (DEHP) is widely being used as product plasticizer like poly-vinyl-chloride (PVC) [1]. This kind of phthalate is easily removed from plastic materials because it lacks covalent bonding with plastic materials due to its weak bonding power; it is easily exposed to humans during the process of production, moving process or process of utilization [2]; and it can also easily be exposed to humans through food, water, meat or any food items that contain phthalates [3].
Phthalates have low acute toxicity [1], but can cause fetal death, deformity, injury of the testicles and liver, and augmentation of oxidizing agents by acting as an endocrine disruptor [4]. Development abnormalities in experiment animals include weight decrease at birth, low survival rate, deformity in genital organs, and decrease in the length of the male genital organ [5]. In addition, in previous studies, Jaakkola et al. [6] suggested that phthalates act as or act similarly to an allergen, and Bornehag et al. [7] proved the relevancy between the concentration of DEHP and butyl benzyl phthalates (BBzP) in dust and allergic disorders. Among studies done in Korea related to phthalate concentration in the environment, Kim et al. [8] monitored phthalates in indoor dust from childcare facilities (19 kindergartens, 21 elementary schools), and from private houses (17 old apartments, and 22 new apartments). Kim et al. also reported investigation results of higher level of DEHP, etc. from childcare facilities (kindergartens 591 µg/g dust, elementary schools 418 µg/g dust) than from private houses (new apartments 259 µg/g, typical apartments 403 µg/g). Study results related to phthalates in indoor dust that have officially been presented are rare. However, there are the results of Yang et al. [9] regarding volatile organic compounds (VOCs) in childcare facilities and indoor-playground, and there are also results of other assessment materials.
It has been reported that incidental dust ingestion is the main route of exposure to phthalates [10,11], and there are many reports that there is higher exposure dosage of phthalates among children than among adults, which is associated with child-specific behaviors in child activity spaces (childcare facilities, houses); namely, crawling, taking child's hand to his mouth and so on [12-15]. However, it is practically difficult to do a standard assessment of exposure to phthalates from child facilities through standard comparison, and it is also difficult to immediately differentiate between the harmful effects of chronic exposure and those of acute exposure. Thus, there are uncertainties due to the various means of exposure, but there should be assessment through health risk. Especially in case of phthalates that lack a standard, one of the ways in which the quantitative assessment of chronic exposure through multipath exposure of pollution materials can be done is through health risk assessment (HRA) [16].
Consequently, children are exposed through main activity spaces such as childcare centers and products within indoor playgrounds. This study aims to identify the exposure route and to estimate the extent of risk due to multi-route exposure of certain phthalates that are child-sensitive materials through health risk assessment.
MATERIALS AND METHODS
I. Selecting Children's Space
This study took in appointed indoor playgrounds (not free of charge) and childcare centers (playrooms, daycare centers, kindergartens). The researchers selected six cities nationwide (Seoul, Ansan, Daejeon, Suwon, Busan, and Yeosu) and investigated 42 indoor playground facilities, 40 playrooms, 42 daycare centers, and 44 kindergartens. Each city had 5-8 places for regional differences.
The first investigation, (in summer) was done through facility arrangement and measurement at the same time during July, August and September of 2007 at the same time. The second investigation, (in winter) was related to exposure assessment done twice, in January and February 2008. In the first and second investigations, identical facilities were investigated repeatedly. The investigation was done in the main play area and the rest area in the case of an indoor playground, and the researchers set a space where study and play was running parallel to the representative point based on class in the case of childcare centers.
Because of the floor dust concentration depending on time and space, the researchers tried to minimize error by measuring the accumulated dust. A previous study [7] suggested main results after having extracted more than fixed indoor floor dust (25 mg). In addition, while arranging the concentration facility, the investigation was done only under the condition that the facilities agree to participate in the research.
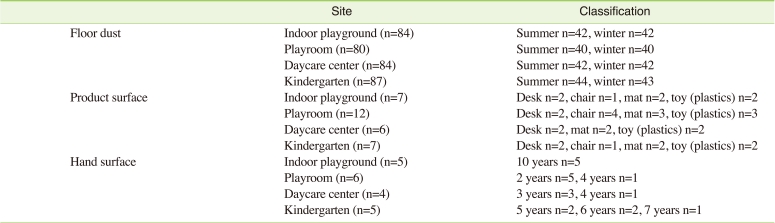
Surface sampling of representative products inside the facilities was executed once, in winter, during January and February of 2008. The product surface samples were extracted from four regions (Seoul, Ansan, Busan, and Yeosu) out of six main investigation regions. In four regions, surface samples were extracted from 3-4 representative product groups (desks, chairs, floor mats, etc.) from each facility, which was categorized as one of four groups (indoor playground, play-room, daycare center, and kindergarten) (Table 1). The representative spaces and items were primarily selected based on the results of questionnaires given to the heads of childcare centers, nursery teachers, and proprietors. From among products within the spaces, the representative products were chosen after having selected products that have high frequency of contact or use up to fourth rank.
II. Measurement of Phthalate
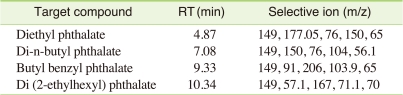
In this study, among all widely used phthalates, the four kinds that are most commonly consumed, used domestically and assessed in former studies [6,12,17] were quantitatively analyzed. These were DEHP, BBZP, diethylphthalate (DEP) and di-n-butyl phthalate (DnBP). In this study, the main exposure media were floor dust, product surfaces and child hand surfaces only.
A vacuum cleaner specifically prepared for sampling indoor dust was used by attaching a filter (Whatman, 125 mm) to the dust collector. In order to avoid any direct exposure to phthalates, filters were stored in a glass dish (130 mm) specially designed for this study. The samples were stored at ambient temperature. After measuring the weight of reagent paper and removing no less than 25 mg of dust [7], the amount of dust prior to examination was weighed. They then took out some of the dust by putting a funnel on a 10 mL bottle after having quantified the amount of dust before treatment, and the sample was extracted via supersonic waves for 30 minutes after soaking the dust with 4 mL of dichloro-methane (DCM, J.T. Baker NJ, USA). The researchers filtered the dust that was extracted by supersonic waves using a filter on a 10 mL bottle. After having concentrated the dust sample using evaporator equipment, they put the sample in a brown bottle used for GC analysis and kept it in a vacuum state in a desiccator for 24 hours. They kept the dust sample refrigerated in vacuum after adding 1mL of methanol. Quantitative analysis was done using a gas chromatograph /mass selective detector (GC/MSD, Agilent Technologies, CA, USA).
In order to do sample extraction of the phthalate product surface sample, the researchers washed their hands with DCM and used gauze (Gauze pad, Sang Kong gauze, Korea). Prior to sample extraction, the gauze was also washed with DCM and covered in foil so that it would not be affected by outside factors. The product surface was then washed 4-5 times using the dry cloth (Cotton Gauze Pads, 10 cm×10 cm). The gauze that was wiped out was kept refrigerated after being placed into a brown glass bottle. The researchers pretreated the sample for analysis by doing extraction using soxhlet equipment for six hours by mixing DCM and acetone solvent (200 mL) at a 1:1 ratio. Using evaporator equipment, the sample was put into a brown bottle for GC analysis after having been concentrated for 50 minutes. After being kept in a vacuum state inside the desiccator for 24 hours, the researcher sealed the sample in 1 mL of methanol and kept it refrigerated. Quantitative analysis was done using GC/MSD.
In case of hand surface samples, the researchers, after washing their own hands in DCM and intercepting the contamination of phthalates, wiped both sample hands after soaking cotton gauze in wet isopropanol 2 mL (50% water solution). The gauze that was used to wipe the sample hands was put inside the brown glass bottle and kept refrigerated. Pretreatment, analysis by machine, and conditioning was carried out in the same way as the product surface sample. Quantitative analysis was done using GC/MSD.
The substance was confirmed using total ion chromatogram (Table 2).
The recovery rate was evaluated by applying identical pretreatment and machine analysis condition using the "standard dust", as suggested by a previous study by Clausen et al. [18], after having inserted the phthalates standard solution in random concentrations.
The recovery rate of phthalates according to medium is dust sample 80-115%, product surface sample 70-95%, and hand surface sample 75-110%. There were differences according to medium, but it was at a level where it could be trusted. The limit of detection (LOD) was LOD = 3 × (detection peak/blank peak + standard deviation [SD] [19]), and the rates of exposure to phthalates were DEHP 0.015, DnBP 0.657, BBzP 0.017 µg/g for the dust samples, and DEHP 0.002, DnBP 0.00002, and BBzP 0.006 µg/cm2 for the product surface and hand surface samples.
III. Statistical Analysis
To assess exposure to phthalates (DEHP, DEP, DnBP, BBzP) per medium, the suggested average, minimum, maximum value, comparison of target child facility and majority group medium, along with statistical significance, were assessed through nonparametric analysis of Kruskal-Wallis test. Statistical analysis was carried out using SPSS version 16.0 (SPSS Inc., Chicago, IL, USA).
IV. Health Risk Assessment
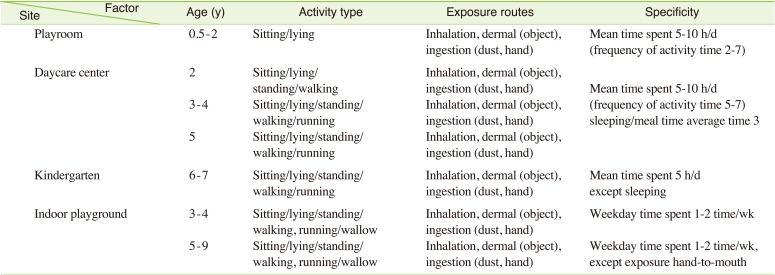
The target facility and age was classified as playroom (0.5-2 years old), daycare center (2-5 years old), kindergartens (5-6 years old), and indoor playground (3-9 years old).
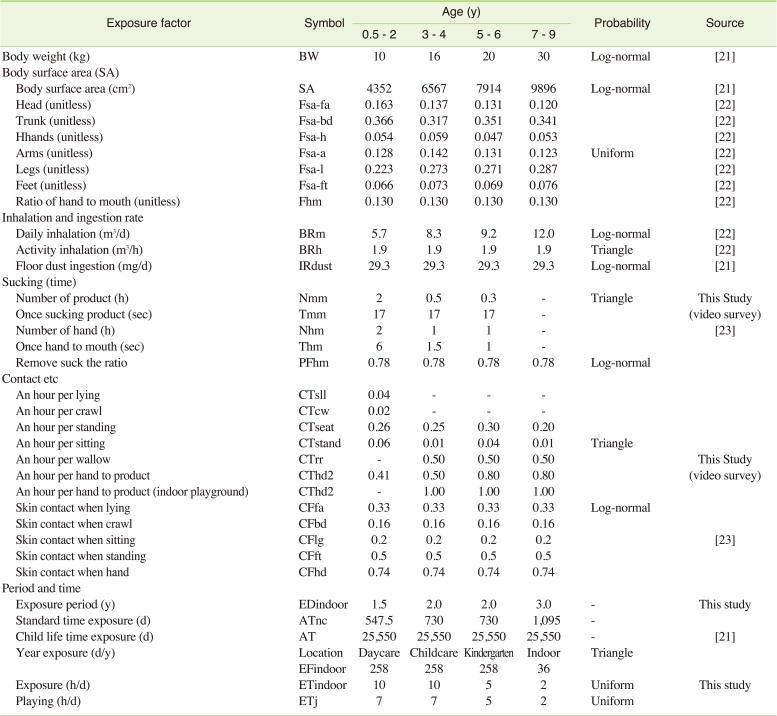
A) Exposure patterns
Using time in each facility and other general information was investigated through a questionnaire and interview form filled out by the nursery teacher. Factor value deduction to calculate the extent of exposure and investigation of exposure configuration analysis was done by separating the subjects into four age groups, and a total of 16 people were investigated. In the case of nurseries, the teacher and head of the nursery did an interview and filled out a questionnaire, and in the case of indoor playgrounds (not free of charge), the facility manager or proprietor did the interview and filled out the questionnaire. The content of the questionnaire and interview questions included general questions related to use of childcare centers and indoor playground, and characteristics and information about child's play (play time, frequency, number of days and hours, etc.).
In order to observe the specific exposure mode in the case of the nurseries, the researchers recorded 40 minutes of free play time by camcorder, with the cooperation of the facility. There were differences according to age, but evidence suggesting that children's activity during free play time is most active and that they show various forms of play led the researchers to decide to observe and record the children during morning free play time. Through interpretation of the video, the researchers judged whether the children's forms of play caused any unique form of exposure in the target space. Forms of play included standing, sitting, walking, running, and rolling around, etc. (Table 3).
B) Dose-response data
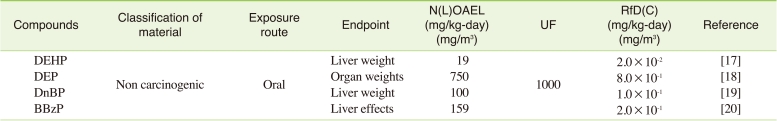
Classification of levels of health risk was done based on toxic effects through infant and childhood period exposure, and then based on carcinogenesis, genital organ toxicity, growth toxicity, nerve toxicity, immune toxicity, and next generation toxicity. The researchers collected data and did an inquiry based on the data that was collected. Through this inquiry, the researchers categorized the substances as carcinogenic or non-carcinogenic, with the latter being substances whose level of toxicity varied according to exposure amount rather than exposure period.
The health risk of the target substance was concluded based on toxicity data officially collected by the Integrated Risk Information System (IRIS) of the Environmental Protection Agency (EPA) and by World Health Organization (WHO). Table 4 shows toxicity data by substance. According to the HRA, if the data was judged to induce sensitive non-carcinogenic toxic effects during the infant and toddler period, and it was categorized as a non-carcinogenic child-sensitive substance.
C) Application of Formula and Factor according to Exposure Scenario
The characteristics of phthalates, including low steam pressure and a high absorption coefficient, their concentration in gaseous state inside indoor atmosphere would be low, and their dust absorption rate would be high [24], so the researchers excluded the possibility of gas inhalation exposure. Skin exposure routes could be through contact with the toy surface, contact with flooring material, and contact with floor mats. Consequently, reflecting the characteristics of childhood exposure, the concentration of floor dust in each facility as well as the representative data for product surface and child hand surface concentration were used when assessing exposure by absorption through ingestion and skin contact. The formulas of particular exposure scenarios related to the data are shown in (1) and (2).
Oral ingestion exposure can occur through hand to mouth behavior via a toy product surface, through hands that are polluted with harmful substances from a floor mat, as well as through ingesting the floor dust. Exposure factors that could be applied to exposure amount calculation were chosen through a literature survey and examined using a questionnaire and observation survey.The researchers established the age of the exposed child by doing a questionnaire. They selected age groups that could comprehensively explain the characteristics of child exposure through their use of certain facilities. Representative formulas per exposure route (1) and (2) as well as calculationson the basis of values used in formulas are suggested in Table 5.

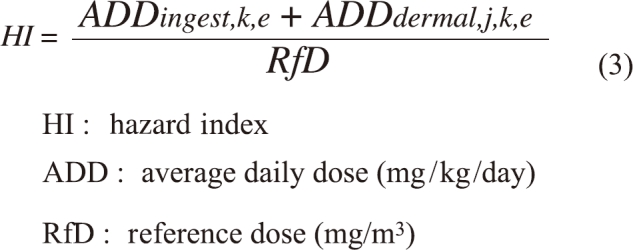
D) Risk calculation
In this study, the target groups were infants (6 months-2 years old), toddlers (3-4 years old), preschool children (5-6 years old), children below the age of 10 attending school (7-9 years old). Health risk was computed according to facilities, substances, and routes of exposure. Child sensitive materials went through the tolerable daily intake (TDI) decision process, and in the case of an absence of TDI, the researchers substituted the reference dose (RfD) value and computed the hazard index (HI). Finally, the HI value was computed as follows (3). Final health risk probability distribution values were obtained by using probability distribution values of ADD according to types of facility, material and age. For assessment, 50% values and 95% values of health risk probability distribution were used, and as a criterion while HI were done by determining whether to exceed 0.1-1.
RESULTS
I. Multi-Route Exposure Assessment
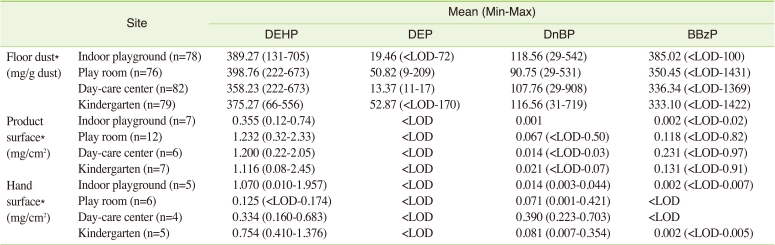
The results of multi-route exposure in child facilities (floor dust, product surface and child hand surface) are shown in Table 6.
In order to determine the concentrations of phthalates in the floor dust (also known as main route of child exposure), the researchers measured the values based on 168 facilities during the summer period and 167 facilities during the winter period. The results were as follows: DEHP was 100%, DnBP was 100%, BBzP was 79.4%, DEP was 6.3%. Except for DEP, all of the substances showed a detection rate of higher than 80%. In the target facilities, DEHP was measured to be, on average, 388 µg/g dust, BBzP was 339 µg/g dust, DnBP was 105 µg/g dust, and DEP was 32 µg/g dust. The order was DEHP> BBzP> DnBP> DEP and there were no significant differences according to substance and facility (p<0.05). This is presumed to originate from the similarities among child facilities.
Table 6 shows the results of assessment of phthalates that came out of product surfaces from each facility. The detection rate of DEHP was 100%, DnBP was 96.9%, and DEP was below the detection limit. DEHP and DnBP showed rather high detection rates in playrooms (1.232 µg/cm2, 0.672 µg/cm2) as compared to other facilities. BBzP, on the other hand showed a higher detection rate in childcare centersthan in other facilities, but the difference was not statistically different (p<0.05).
Table 6 shows the results of the assessment of phthalates from hand surfaces per facility. DEHP and DnBP showed high detection rates of 100%, BBzP was 45.0%, and DEP was below the detection rate. DEP was not detected on hand surfaces in any facility, DEHP was 1.070 µg/cm2, DnBP in childcare centers was 0.390 µg/cm2, and BBzP was 0.002 µg/cm2 in kindergartens, showing a higher average than in other facilities. The difference was not statistically significant (p<0.05). Although it is not shown in our study tables, the exposure results even according to regions and seasons did not show any statistical difference. In the case of dust, this is judged to have resulted from not being able to chase after difference from each facility due to pollutant sources related to the products, and in the case of other samples, this is judged to have resulted from having a limited number of samples.
II. Health Risk Assessment
The researchers gathered information on target substance, age groups, exposure factor and exposure scenario of child sensitive impact substance and computed HI; these levels are shown in Table 7.
After considering the physiological and behavioral characteristics of children, and after having calculated the HI of non-carcinogenic toxic phthalates, they didn't find any substance or facility that exceeded 0.1. The 50th percentile value (middle value) of HI through DEHP exposure was playroom 0.005, daycare center 0.007, kindergarten 0.003, indoor playground (not free of charge) below 0.001; for the 95th percentile value, play-room was 0.014, daycare center 0.017, kindergarten 0.008 and indoor playground was below 0.001.
In case of playrooms, phthalate exposure rate was 79.7% ingestion exposure and 20.3% skin exposure, and it was found that exposure through floor dust ingestion was the main route (dust 88.5%, product 10.5%, hand 1.0%). In the case of childcare centers, 67.6% of exposure occurred through the ingestion route and 32.4% through skin exposure, and it was found that exposure through floor dust ingestion was the main route (dust 62.6%, product 29.3%, hand 8.1%). In the case of kindergartens, the ingestion route accounted for 76.5% and skin exposure for 23.5%, and it was found that exposure through floor dust ingestion was the main route (dust 76.5%, product 8.2%, hand 15.4%). In case of indoor playgrounds (not free of charge), the ingestion route exposure accounted for 84% and the skin exposure route for 16%, and floor dust ingestion exposure was the main route (dust 79.3%, product 14.1%, hand 6.6%).
DISCUSSION
Phthalates are more affected through indoor product discharge than through outdoor effect, and the seasonal effect does not lead to exposure to phthalates because phthalates have a low steam pressure and have a high absorption coefficient by nature. In terms of seasons, comparing summer, which has a wet season that affects indoor water leakage [24], with dry winter, the researchers determined the concentration of phthalate distribution in the floor dust in order to find out the extent of exposure within the environment. The most significant medium of inhalation was through indoor air or indoor dust, but because the exposure effect within the atmosphere was insignificant in the former studies [25-28], exposure through ingestion of phthalates included in indoor dust was very important. Koch et al. [29,30] reported that 75% of DEHP exposure is through oral ingestion. Normally, it is reported that the most important source of exposure to DEHP is through food, and Meek and Chan [31] calculated daily exposure of DEHP to be 10 µg/kg/day. For exposure through toys, the researchers presumed 5.7-44 µg/kg/day through the behavior of hand-to-mouth activity.
When considering previous data on floor dust, which is the main source of exposure, Clausen et al. [25] reported the average concentration in a Denmark general household (n=23) to be 858 µg/g DEHP dust, and Bornehag et al. [24] has previously reported concentration of DEHP in the dust of a child's bedroom (n=346) in a general household in Sweden as 770 µg/g. Fromme et al. [32] mentioned that DEHP makes up 80% of phthalates in indoor dust in general households. Even in this research, the composition ratio revealed DEHP to have the highest concentration. In this research, DEHP has the highest composition ratio, but it is notable that there was higher composition ratio of BBzP than in studies done by other countries. A person can be exposed to BBzP through carpet, PVC flooring material and vinyl wallpaper [8]. Therefore, the results seem to have been affected by a high rate of usage of floor mats, flooring material, and vinyl wallpaper inside child-targeted facilities [32].
Phthalates are judged to be substances that have multipath/multimedia exposure through all routes including indoor floor dust, product surface, and inhalation; through a child's hand, skin contact, and dust ingestion. Phthalates or any placticizers do not chemically bond with PVC [1]. The older the building is, the higher the possibility that phthalates could be discharged from flooring or building material. However, in this research, no clear result was found due to the effects of various toys, desks, chairs, and study materials. According to Bornehag et al. [24], preventive measures need to be taken inside child-targeted facilities due to leakage of water causing humidity, possible additional exposure due to low performance of PVC flooring material.
This study included an actual survey of playrooms, daycare centers, indoor-playgrounds and kindergartens from six cities, but these facilities cannot represent all domestic facilities. In the case of indoor playgrounds especially, the researchers only measured those that are not free of charge; data on free indoor playgrounds that are managed individually could not be included. Also, due to limits such as active space assistance, representative facility sample extraction (area, construction year, location, etc.) according to population distribution did not happen. There were limitations, such as representativeness of actual survey because of one-time measurement done by season, and in the case of product surfaces and hand surfaces, sampling of other metals, and pesticides were running parallel to phthalates sampling, so not too many samples could be extracted.
These points need to be supplemented with research that have continuity later on, and these points are meaningful for being an exemplary research while there are not many studies done on exposure to phthalates.
CONCLUSION
Considering the physiological and behavioral characteristics of children who use the target facilities, after evaluating the risk level of non-carcinogenic toxicity of phthalates, there was not substance or facility that exceeded the HI 0.1 level. When looking at the contribution rate of phthalates exposure according to the routes in the playrooms, daycare centers, kindergartens, and indoor playgrounds (not free of charge), exposure through ingestion was 67.6-84.0%, skin exposure was 20.3-32.4%, and it was found that exposure through floor dust was the main route of exposure to the phthalates. Phthalates, based on this research, are steadily found in all media (indoor dust, product surface, hand).
ACKNOWLEDGEMENTS
This study was a part of project supported by Korean Ministry of Environment (Environmental Health Policy Division Office of Environmental Health), "Risk Assessment in Facilities for Child" ('07-'08).
Notes
The authors have no conflict of interest to declare on this study.
This article is available from: http://e-eht.org/