AbstractObjectivesWe aimed to investigate the acute effects of heat stress on body temperature and blood pressure of elderly individuals living in poor housing conditions.
MethodsRepeated measurements of the indoor temperature, relative humidity, body temperature, and blood pressure were conducted for 20 elderly individuals living in low-cost dosshouses in Seoul during hot summer days in 2010. Changes in the body temperature, systolic blood pressure (SBP) and diastolic blood pressure (DBP) according to variations in the indoor and outdoor temperature and humidity were analyzed using a repeated-measures ANOVA controlling for age, sex, alcohol, and smoking.
ResultsAverage indoor and outdoor temperatures were 31.47℃ (standard deviation [SD], 0.97℃) and 28.15℃ (SD, 2.03℃), respectively. Body temperature increased by 0.21℃ (95% confidence interval [CI], 0.16 to 0.26℃) and 0.07℃ (95% CI, 0.04 to 0.10℃) with an increase in the indoor and outdoor temperature of 1℃. DBP decreased by 2.05 mmHg (95% CI, 0.05 to 4.05 mmHg), showing a statistical significance, as the indoor temperature increased by 1℃, while it increased by 0.20 mmHg (95% CI, -0.83 to 1.22 mmHg) as outdoor temperature increased by 1℃. SBP decreased by 1.75 mmHg (95% CI, -1.11 to 4.61 mmHg) and 0.35 mmHg (95% CI, -1.04 to 1.73 mmHg), as the indoor and outdoor temperature increased by 1℃, respectively. The effects of relative humidity on SBP and DBP were not statistically significant for both indoor and outdoor.
INTRODUCTIONThe surface air temperature has increased significantly by about 1.5℃ during the past 100 years on the Korean peninsula which is higher than the global average increase of 0.74℃ [1]. Given the increase in the frequency and intensity of extreme weather events such as heat waves predicted in the future due to climate change [2], a number of researchers have drawn attention to the effects of external temperatures on human health and have characterized vulnerable groups [3-13].
Low-income groups are highly vulnerable to extreme weather events such as high temperatures and natural disasters [3,4]. Naughton et al. [5] reported that air-conditioners are the strongest protective factor against heat-related death, showing that low-income groups can be very vulnerable to the effects of high temperature. Poverty can be a risk factor for heat-related illnesses and deaths because the poor are more likely to live in heat-island urban areas [6] and are less likely to be able to afford air-conditioning [7-9].
In addition, it is well known that elderly people do not adjust compared to young people to sudden changes in temperature because they are more likely to have a chronic medical condition that changes normal body responses to heat [9-13]. The most serious short-term effects of excessive environmental heat are caused by the impact on the body's thermo-regulating mechanism, water and electrolyte balance, and the increased demands imposed on the cardiovascular system [13], which means that elderly people may be much more susceptible to heat stress than younger people because they are more likely to have cardiovascular diseases. Previous studies [14,15] reported that elderly persons may be particularly susceptible to temperature-related variations in blood pressure. The baroreflex, which is one of the mechanisms of blood pressure regulation, is modified in elderly subjects [14]; it has been hypothesized that disorders of baroreflex control and enhanced vasoreactivity could contribute to the aging-associated increase in cardiovascular morbidity [15].
Although both poverty and old age are critical risk factors for heat-related illness and death, there are few studies on the health effect of heat waves on the poor and elderly people. Kim and Joh [3] studied the effect of high temperatures on low-income elderly people in terms of excess mortality due to heat stress. However, their study did not include changes in physical condition and the disease burden.
In order to reduce the adverse health impact of extreme hot weather, potential health effects should be predicted based on an understanding of vulnerable groups who are susceptible to climate change. One of the best ways to predict potential health effects of heat stress on the elderly living in poor conditions is to measure the changes in primary outcomes, including the blood pressure and body temperature, caused by the hot weather. This would lead to a better understanding of the health effects of climate change and would allow the formulation of an adaptation strategy considering the socioeconomic status of people.
The purpose of this study is to investigate the indoor environmental climate of dosshouses and to assess the acute effects of heat stress on body temperature and blood pressure in elderly individuals living in poor housing conditions.
METHODS AND MATERIALSI. Study DesignFor this study, we surveyed elderly individuals living in dosshouses, called zzockbang in Korean, which literally means a very small room divided into several compartments, each allowing just one individual, in Donui-dong, Jongno-gu, Seoul, Korea. Residents living in dosshouses have no personal kitchen or bathroom and many dosshouses have no windows. In metropolitan Seoul, there are five large slum areas. Among them, the Donui-dong zzockbang area, with about 500 residents, is located in the center of Seoul and is surrounded by large tall buildings and crowded streets, meaning that the area easily becomes a heat island in summer.
Dosshouses in slum areas are mainly occupied by elderly individuals of low socioeconomic status who typically live alone. As the sizes of the dosshouses are very small with no air-conditioning, it was predicted that the people living in these houses would be directly exposed to heat waves during hot summer days. Twenty elderly persons who agreed to participate in our survey were selected for repeated measurements of their body temperature and blood pressure.
The survey was carried out between July 27 and August 6, 2010. The summer of 2010 was one of the hottest summers in Korea. There were 12.2 tropical nights on the average of whole country in August, which is 6.5 days more than the average of the most recent 10 years (2001-2010). From August 1 to August 6, 117 of patients were diagnosed as suffering from hyperthermia (45 % of hyperthermia patients in 2010). 4 cases died due to heat wave during the same time among the 8 cases which occurred in 2010 [16].
We collected two types of data: climatic variables such as temperature and humidity and health indicators such as body temperature and blood pressure through repeated measurements. In addition, we surveyed the housing conditions, the self-reported health outcomes during successive days of hot weather, and the behavioral habits of the participants to adjust for confounding factors.
We then analyzed changes in the body temperature, systolic blood pressure (SBP) and diastolic blood pressure (DBP) according to variations in the indoor and outdoor temperature and humidity using a repeated measures ANOVA controlling for age, sex, alcohol and smoking.
II. Personal Exposure MeasurementsThe indoor temperature and humidity of the dosshouses during the survey period were measured with an electronic hygrothermograph (AE-817CE, B&J, China). For the calibration of the thermometer and hygrometer used in the study, the researchers installed a total of 20 thermometers and hygrometers in the same indoor space, stabilized them for 40 minutes, and measured device-specific values a total of five times at 15-minute intervals. Variations were revised based on the wet-bulb globe temperature (WBGT; QUESTtemp°30, Quest® Technologies, Oconomowoc, WI, USA) levels measured at the same location. Calibrated thermometers and hygrometers for every household, installed to avoid particular heat source locations, were used to measure the temperature and relative humidity in the morning (8:00-9:00) and afternoon (14:00-15:00) during the study period. In addition, the temperature and humidity values were recorded hourly over nine days in two households that participated in the study.
For the outdoors, the hourly temperature and three-hourly relative humidity data were obtained from the Korea Meteorological Administration. We collected the data measured in Songwoll-dong Jongno-gu, Seoul, which is the nearest station to the study area, located at 37.34°N and 126.57°E. For temperature, we utilized the average of 8 am and 9 am data for morning and of 2 pm and 3 pm data for afternoon. For relative humidity, we adopted the 9 am and 3 pm data for morning and afternoon from among the three-hourly data sets, respectively. Discomfort index (DI) was also calculated based on the measured indoor temperature and relative humidity. We adopted the formula proposed by Thom [17]. The formula used is as follows:
DI=9/5×Ta - 0.55×(1-RH)(9/5×Ta - 26)+32
where DI is the discomfort index; Ta indicates the dry-bulb temperature; and RH is the relative humidity.
After a full five minutes of rest, seated blood pressure and body temperature were measured by trained research assistants twice a day in accordance with the time when the meteorological data were measured. Blood pressure measurements were recorded in parallel using a mercury sphygmomanometer on meter on the right arm using appropriate cuff sizes. Body temperature was also measured using Braun ThermoScan IRT-4520 ear thermometer twice a day at the same time as the blood pressure measurements.
It would have been better to measure the hourly indoor temperature and to make more frequent measurements of health indicators for a more delicate assessment of relationship between indoor climatic variables and health indicators. However, due to poor security, like most slum areas, it was impossible to measure these factors more frequently, especially at night.
III. Statistical AnalysisChanges in the body temperature, SBP and DBP according to variations in the indoor and outdoor temperature and humidity were analyzed using a repeated measures ANOVA controlling for age, sex, alcohol and smoking. Repeated measures ANOVA, a type of mixed effect model, compares the average score at multiple time periods for a single group of subjects. The data in this case were collected over time; specifically there were 18 repeated measurements for each subject during the study period. To reduce the bias between subjects, a random effect was adopted for the subject. For covariance parameters, we used a first-order autoregressive [AR(1)] covariance structure, which has homogeneous variances and correlations that decline exponentially with the distance, considering that the repeated measurement data are generally associated with autoregression owing to the narrow time interval.
The model specifications we used are as follows:
Yij=β0+β1(TEMP)i+β2(RH)i+β3Xi+…+βnXni+ξij+eij
where β0 is the overall intercept; β1 is the coefficient of the exposure to temperature (TEMP); β2 is the coefficient of the relative humidity (RH); β3…βn are the coefficients for the covariates included in multivariate models; ξij denotes the random effect for the subject; j represents the subject; i represents the measurement time, and eij is the residual error term. All tests were two-sided, and an alpha level of less than 0.05 was considered significant. In the model for body temperature, sex and age were included, and in case of blood pressure, sex, age, current smoking habit, alcohol consumption, and measurement time (morning and afternoon) were included for adjustment. In the models for the DI, indoor DI was included instead of the indoor temperature and indoor relative humidity and same covariates were considered for the body temperature and the blood pressure models.
The statistical package SAS version 9.2 (SAS Inc., Cary, NC, USA) was utilized to complete the statistical analysis.
RESULTSI. Summary of Subjects
Table 1 shows the summary statistics of the subjects including their demographic characteristics, meteorological data, and health indicators as measured during the study period. The average age of the participants was 74.3 (standard deviation [SD], 8.2) years. Three (15.0%) of 20 elderly people were current alcohol drinkers and nine (45.0%) had a habit of smoking.
The indoor temperature of the dosshouses was 31.5℃ (SD, 1.0℃) on average while the outdoor temperature for the same time, as measured by the Korea Meteorological Administration, was 28.2℃ (SD, 2.0℃), showing that the indoor temperature of the dosshouses was 3.3℃ higher overall.
The indoor relative humidity of the dosshouses was 73.7% (SD, 6.7%) on average while the average outdoor relative humidity for the same time was 68.4% (SD, 12.6%). Compared to outdoors, there was less variation in both the indoor temperature and the humidity, which means that the hot and humid indoor condition was maintained during the study period without falling. The indoor DI was 84.2 (SD, 1.8) on average, showing that the indoor area was very uncomfortable for the residents.
The body temperature of the participants was 36.5℃ (SD, 0.4℃) on average and the SBP and DBP were respectively 133.66 mmHg (SD, 24.5 mmHg) and 81.68 mmHg (SD, 15.3 mmHg).
Figure 1 shows the comparison of the daily indoor temperature and relative humidity in the dosshouses with the outdoor condition in Jongno-gu, Seoul, from July 27 to August 6, 2010. All values for the indoor temperature of the dosshouses were higher than those of outdoor area; the average indoor temperature at 8-9 am for 9 days was 31.1℃ (30.5-32.1℃), while the average outdoor temperature at 8-9 am for the same period was 26.6℃ (25.4-28.8℃). The average indoor temperature at 2-3 pm for 9 days was 31.9℃ (31.1-32.8℃), while the average outdoor temperature at 2-3 pm for the same period was 29.9℃ (28.0 - 32.1℃). In particular, the temperature difference in the morning was higher than the difference in the afternoon, and was about 4.6℃ higher than the air temperature in Jongno-gu, Seoul during these two times. Furthermore, the tropical night phenomenon, nights with a minimum temperature exceeds 25℃, occurred every day from July 30 to August 6, 2010 except for August 3.
There was little difference between the indoor and outdoor relative humidity in the morning; the average relative humidity of indoors was 75.4% (67.0-82.6%) and that of outdoorswas 76.0% (66.0 - 93.0%). However, for the afternoon (2-3 pm), the indoor relative humidity was much higher than the outdoor reading; the average indoor relative humidity at 2-3 pm for 9 days was 72.0% (63.0-78.9%), while the average outdoor relative humidity was 60.0% (34.0-73.0%), showing more variation by date.
II. CorrelationThe correlation coefficients of the body temperature related to the indoor and outdoor temperature and the indoor DI were 0.310, 0.231, and 0.261, showing a positive significant relationship.
For the blood pressure readings, both the SBP and the DBP showed a significantly negative relationship with the indoor temperature and the DI, presenting values of -0.243 and -0.280, respectively, for the indoor temperature and -0.178 and -0.145, respectively, for the DI, whereas they presented no significant correlation with the outdoor temperature. The body temperature and blood pressure showed no significant correlation with the indoor or the outdoor relative humidity.
III. Effects of Meteorological Variables on Health IndicatorsThe effects of the temperature and humidity on the body temperature and blood pressure are given in Table 3. The body temperature increased by 0.21℃ (95% confidence interval [CI], 0.16 to 0.26℃) and 0.07℃ (95% CI, 0.04 to 0.10℃) as the indoor and outdoor temperature increased by 1℃ with the adjustment of age and sex. The body temperature also increased by 0.08℃ (95% CI, 0.05 to 0.11℃) with an indoor DI increase of 1℃. However, the effects of the relative humidity on the body temperature were not statistically significant for both indoor and outdoor readings.
The SBP decreased by 1.75 mmHg (95% CI, -1.11 to 4.61 mmHg) and 0.35 mmHg (95% CI, -1.04 to 1.73 mmHg) as the indoor and outdoor temperature increased by 1℃, respectively. It also decreased by 0.76 mmHg (95% CI, -0.60 to 2.11 mmHg) with the indoor DI increase of 1℃ when age, sex, smoking, alcohol, and morning and afternoon were controlled as confounding factors.
The DBP decreased by 2.05 mmHg (95% CI, 0.05 to 4.05 mmHg), showing statistical significance, as the indoor temperature increased by 1℃, while it increased by 0.20 mmHg (95% CI, -0.83 to 1.22 mmHg), showing with no significance, as the outdoor temperature increased by 1℃. The DBP decreased by 0.11 mmHg (95% CI, -0.87 to 1.09 mmHg) with an indoor DI increase of 1℃, although this was not statistically significant.
While the SBP decreased by 0.05 mmHg (95% CI, -0.28 to 0.39 mmHg), the DBP increased by 0.22mmHg (95% CI, -0.46 to 0.02 mmHg) with an increase in the indoor relative humidity of 1%, showing no significance.
We compared the effect of climatic variables on the body temperature and blood pressure between a hypertensive elderly group and a non-hypertensive group. The hypertensive group was defined as subjects who had been diagnosed as suffering from hypertension by a doctor and who were taking an anti-hypertension drug. Nine (45.0%) of 20 elderly peoplewere classified as hypertensive group. Upon analyzing the hypertensive and non-hypertensive subjects separately, the SBP of the hypertension group was found to increase by 3.18 mmHg (95% CI, -2.20 to 8.55 mmHg), showing no statistical significance, while the DBP of the hypertension group decreased by 0.69 mmHg (95% CI, -3.32 to 4.70 mmHg) as the indoor temperature rose by 1℃. However, the SBP of the non-hypertension group decreased by 3.17 mmHg (95% CI, -0.23 to 6.57 mmHg), showing no statistical significance, as the indoor temperature rose by 1℃. The DBP of the non-hypertension group decreased by 1.43 mmHg (95% CI, 0.81 to 3.67 mmHg). The effects of relative humidity on blood pressure were not significant in both hypertension and non-hypertension groups. The body temperature of the hypertension group increased by 0.26℃ (95% CI, 0.17 to 0.35℃) and that of non-hypertension group increased by 0.19℃ (95% CI, 0.12 to 0.25℃) as the indoor temperature rose by 1℃ showing statistical significance (Table 4).
DISCUSSIONWe investigated the indoor environmental climate of dosshouses located in the center of metropolitan Seoul during hot summer days to assess their health impact on those whose health was most likely to be affected by weather-related changes, i.e., elderly people who lived alone in poor housing conditions.
According to the definition of a previous study [18], heat waves were categorized by intensity and duration. Hajat et al. [18] considered 6 heat wave types: periods of 2 or more or 4 or more days of continuous temperatures that are more than the 98.5th, 99th, or 99.5th percentile of the community's temperature distribution. Considering that the average temperature of Seoul is 12.9℃ (SD, 10.2℃) for the last ten years, 2001-2010, and that the 99th and 98.5th percentiles of the average temperature in Jongno-gu, Seoul are 28.6℃ and 28.3℃, respectively, a heat wave was occurred in the study period. The ambient average temperatures of August 5 and 6 in 2010 were 29.2℃ and 28.3℃, respectively, thus matching or exceeding 28.3℃ and having occurred continuously. Furthermore, considering the indoor temperature, the residents in the dosshouses were under a heat wave during all the study period because the daily indoor temperatures were always over 28.6℃, the 99th percentile of the last ten years, showing a range of 29.1-34.8℃ (Figure 1). During the hot days, the indoor DI was very high, showing an extremely uncomfortable condition. That is, the average discomfort index was 84.22 (SD, 1.77), which was higher than the level of 80 at which most people complain of discomfort (Table 1). The average morning and afternoon temperatures were 31.1℃ (SD, 0.8℃) and 31.9℃ (SD, 1.0℃), respectively, and there were not significant differences between them. In Korea, when comparing the air temperature in the summer under the same conditions, the appropriate indoor cooling temperature is suggested to be between 26 to 28℃. Therefore, based upon this information, people residing in dosshouses live in temperatures 4 to 5℃ higher than the advised standard indoor temperature in the summer. According to the records of the hourly room temperature of two participants, the room temperature was comparatively constant regardless of the daily time, having remained at more than 30℃ (Appendix 1). That is, the high temperature lasted all night, which means that the residents in the dosshouses were directly exposed to the high temperature and tropical night phenomenon during the hot summer days.
Dosshouses, with an average room size of 5.1 m2 (SD, 3.5 m2) according to the measurements of 19 dosshouses and without window in half of them, are characteristically clustered together in a narrow space comparable to a labyrinth, which inhibits ventilation and air circulation. Furthermore, residents in dosshouses typically cook in their room using a potable burner and an electric cooker because they have no separate kitchen. This can cause the temperature to rise in the dosshouses during the day. The small building fronts could also lead to less heat escaping, even at night. In addition, due to poor security at the dosshouses, the residents could neither open their doors nor their windows at night, which exacerbated the high-temperature condition.
The rise in body temperature was significantly associated with indoor and outdoor temperature rises (Table 3). The rise in body temperature was more affected by the indoor temperature (0.21℃ of increase in the body temperature per 1℃ increase in the ambient temperature increase) than the outdoor temperature (0.07℃), which reflects the fact that the residents spend most of their time in the dosshouses due to the general difficulty they experience when moving. In addition, the effect of the temperature on the body temperature was higher in hypertensive subjects than non-hypertensive subjects (Table 4).
In order for the human body to maintain a consistent temperature, a continuous exchange of heat with the environment is necessary according to the law of thermodynamics. Body heat is primarily produced through a metabolic process in the interior of the body, and heat exchange between the body and the exterior environment is accomplished through mechanisms such as conduction, convection, radiation, and evaporation. However, when a body is exposed to high temperatures for an extended period, body temperature regulation is inhibited as heat exchange cannot occur properly. Furthermore, the failure of thermoregulation caused by extremely high temperatures may be impaired by dehydration, salt depletion, and increased surface blood circulation [19].
As a consequence of impaired body temperature regulation, our subjects experienced a significant increase in body temperature during the hot days, and at worst some had a slight fever. In addition, a high level of subjective symptoms such as muscle pain, headaches, movement disorders, and difficulty in breathing were also reported; two participants experienced dyspnea, one participant experienced nausea, five participants experienced headache, and six participants experienced muscle aches and stiffness. In addition, during periods of sultry weather, over 50% of the research subjects complained of sleeping disorders; subjects were able to sleep only one third of their normal sleep hours as the average number of sleep hours during the research period was 2.5 compared to the normal sleep hours of 7.4 according to their self-reports.
Some previous studies [20-22] reported that both hyperthermia and hypothermia are generally linked to cardio-respiratory morbidity or mortality. After examining the functions of the cardiovascular, cerebrovascular, and respiratory systems at high temperatures, Michelozzi et al. [23] reported that elderly women had a 4.5% decrease in function per 1℃ increase in body temperature. Therefore, an increase in the body temperature in the poor and elderly can be a potential risk factor to aggravate cardiovascular, cerebrovascular, and respiratory diseases. 21% of the residents living in dosshouses in Korea have one ailment among hypertension, respiratory, and cardiovascular disease [24].
The blood pressure showed a tendency to decrease in relation to indoor and outdoor temperature increases except for the effect of outdoor temperature on the DBP. These results are in good agreement with previous research results related to blood pressure changes according to the season, with one finding reporting that the blood pressure in summer is lower than that in winter [25,26]. In summer, the blood pressure is lower because the veins of the skin expand in order to diffuse body heat. The change in the blood pressure is more obvious among the elderly, and people who are thin react more sensitively to this change. Upon comparing our research results to those of a study that investigated the effect of a change in the temperature on the blood pressure among young adults in Korea [27], which reported that the SBP and DBP decreased by 0.659 mmHg and 0.368 mmHg, respectively, due to a 1℃ increase in the ambient temperature, the effect of the outdoor temperature on the SBP of the elderly people living in the dosshouses was in accordance with findings of the previous research. However, that on the DBP of the elderly people living in the dosshouses was different from the previous study (Table 3); the DBP of the elderly people in the dosshouses increased by 0.20 mmHg due to a 1℃ increase in the ambient temperature although our results were not statistically significant due to the smaller sample size.
The impact of the indoor temperature on the blood pressure was higher than that of the outdoor temperature; the effect of the indoor temperature on the SBP was about 5.1 times of that of the outdoor temperature. In addition, the effect of the indoor temperature on the DBP was statistically significant while that of outdoor temperature was not (Table 3). It can be inferred that the change of the blood pressure is related more to the indoor temperature than to the outdoor because the residents in the dosshouses spent most of their time indoors. Correlation coefficients between the blood pressure and temperature also support this assumption (Table 2).
Alpérovitch et al. [28] pointed out that because decreased blood pressure can be a risk factor for increased mortality in persons who have environmental hyperthermia, the decrease of blood pressure in the elderly people could be an important consideration during a heat wave. they reported that in August of 2003, there was an unprecedented heat wave in France that resulted in approximately 15,000 deaths, mainly of the elderly. After their second follow-up examination of the blood pressure of the affected participants, they also reported that the seasonal fall in the blood pressure values was sharper in August of 2003 (mean SBP, 132 mm Hg) than in August of 2004 (138 mm Hg) [28]. In addition, it is estimated that a decrease in the blood pressure among the elderly due to high temperatures increased the risk of fainting, heat fatigue, and death related to intense heat. This is also likely to be related to deaths caused by hypertension that occur frequently in the summer time [29]. Therefore, attention should be paid on the acute changes in the blood pressure during hot summer days.
This research has limitations, including the fact that we used a relatively small sample size. Considering the problem with public security, the tropical night phenomenon and an assessment of health during the affected times was not included. In addition, the data used in the current study contain some bias, including measurement error such as that caused by differences between the nurses measuring the blood pressure. Despite these limitations, this study is meaningful in that it is the first to assess the effect of a heat wave on the health indicators of elderly people living in extremely poor housing condition as well as to investigate the indoor environmental climate of dosshouses. It is expected that these research results can be used as basic data to construct heat wave adaptive plans that are differentiated and actualized in terms of age and region. In addition, this research can contribute to climate change vulnerability assessments that can be used to minimize the detrimental health effects of heat waves.
In conclusion, the poor and elderly are directly exposed to heat wave both night and day during hot summer days. In a poor housing condition, their vital signs respond sensitively to indoor temperature increase. As weather changes accelerate, it is predicted that the occurrence of heat waves in the summer will increase; thus, more substantial and systematic investigations of the health effects on elderly populations during the heat wave season are needed. In addition, careful adaptation strategies as regards to climate change are required considering the socioeconomic status of at risk groups.
ACKNOWLEDGEMENTSThe authors thank the fieldwork team, especially students from Haja Production School and the Department of Nursing, Eulji University. The authors also appreciate the assistance of members of the Counseling Center for Donui-dong Shelter.
References1. National Institute of Environmental Research, Ministry of Environment. Korean climate change assessment report 2010: technical summary. 2010. Seoul: National Institute of Environmental Research, Ministry of Environment; p. 89.
2. Intergovernmental Panel on Climate Change. Climate change 2007: synthesis report. cited 2012 Mar 12. Available from: http://www.ipcc.ch/publications_and_data/publications_ipcc_fourth_assessment_report_synthesis_report.htm.
3. Kim Y, Joh S. A vulnerability study of the low-income elderly in the context of high temperature and mortality in Seoul, Korea. Sci Total Environ 2006;371(1-3):82-88. 17007909.
4. World Health Oragnization. The world health report 2002: reducing risks, promoting healthy life. cited 2012 Mar 12. Available from: http://www.who.int/whr/2002/en/.
5. Naughton MP, Henderson A, Mirabelli MC, Kaiser R, Wilhelm JL, Kieszak SM, et al. Heat-related mortality during a 1999 heat wave in Chicago. Am J Prev Med 2002;22(4):221-227. 11988377.
6. Lee DH. Seventy-five years of searching for a heat index. Environ Res 1980;22(2):331-356. 7408825.
7. O'Neill MS, Zanobetti A, Schwartz J. Disparities by race in heat-related mortality in four US cities: the role of air conditioning prevalence. J Urban Health 2005;82(2):191-197. 15888640.
8. Curriero FC, Heiner KS, Samet JM, Zeger SL, Strug L, Patz JA. Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol 2002;155(1):80-87. 11772788.
9. Díaz J, García R, Velázquez de Castro F, Hernández E, López C, Otero A. Effects of extremely hot days on people older than 65 years in Seville (Spain) from 1986 to 1997. Int J Biometeorol 2002;46(3):145-149. 12194008.
10. Bell ML, O'Neill MS, Ranjit N, Borja-Aburto VH, Cifuentes LA, Gouveia NC. Vulnerability to heat-related mortality in Latin America: a case-crossover study in Sao Paulo, Brazil, Santiago, Chile and Mexico City, Mexico. Int J Epidemiol 2008;37(4):796-804. 18511489.
11. Kim YM, Kim S, Cheong HK, Kim EH. Comparison of temperature indexes for the impact assessment of heat stress on heat-related mortality. Environ Health Toxicol 2011;26: e2011009. 22125770.
12. Schwartz J. Who is sensitive to extremes of temperature?: A case-only analysis. Epidemiology 2005;16(1):67-72. 15613947.
13. Fish PD, Bennett GC, Millard PH. Heatwave morbidity and mortality in old age. Age Ageing 1985;14(4):243-245. 4036733.
14. Lindgren K, Hagelin E, Hansén N, Lind L. Baroreceptor sensitivity is impaired in elderly subjects with metabolic syndrome and insulin resistance. J Hypertens 2006;24(1):143-150. 16331112.
15. Lipsitz LA, Iloputaife I, Gagnon M, Kiely DK, Serrador JM. Enhanced vasoreactivity and its response to antihypertensive therapy in hypertensive elderly women. Hypertension 2006;47(3):377-383. 16446396.
16. National Emergency Management Agency (NEMA). Comprehensive analysis of disaster situation. 2011. Seoul: NEMA; (Korean).
18. Hajat S, Armstrong B, Baccini M, Biggeri A, Bisanti L, Russo A, et al. Impact of high temperatures on mortality: is there an added heat wave effect? Epidemiology 2006;17(6):632-638. 17003686.
20. González-Alonso J, Calbet JA. Reductions in systemic and skeletal muscle blood flow and oxygen delivery limit maximal aerobic capacity in humans. Circulation 2003;107(6):824-830. 12591751.
21. Braga AL, Zanobetti A, Schwartz J. The effect of weather on respiratory and cardiovascular deaths in 12 U.S. cities. Environ Health Perspect 2002;110(9):859-863.
22. Kunst AE, Looman CW, Mackenbach JP. Outdoor air temperature and mortality in The Netherlands: a time-series analysis. Am J Epidemiol 1993;137(3):331-341. 8452141.
23. Michelozzi P, Accetta G, De Sario M, D'Ippoliti D, Marino C, Baccini M, et al. High temperature and hospitalizations for cardiovascular and respiratory causes in 12 European cities. Am J Respir Crit Care Med 2009;179(5):383-389. 19060232.
24. Korea Center for City and Environmental Research (KOCER). Study on the stabilization policy for poor houses II: understanding the residential environment of dosshouses and the preparation of stabilization policy for housing. 2005. Seoul: KOCER; (Korean).
25. Brennan PJ, Greenberg G, Miall WE, Thompson SG. Seasonal variation in arterial blood pressure. Br Med J (Clin Res Ed) 1982;285(6346):919-923.
26. Minami J, Ishimitsu T, Kawano Y, Matsuoka H. Seasonal variations in office and home blood pressures in hypertensive patients treated with antihypertensive drugs. Blood Press Monit 1998;3(2):101-106. 10212338.
27. Kim JY. Association of weather variables with health outcome [dissertation]. 2010. Seoul: Seoul National University; (Korean).
Table 3Effect of temperature and humidity on body temperature and blood pressure 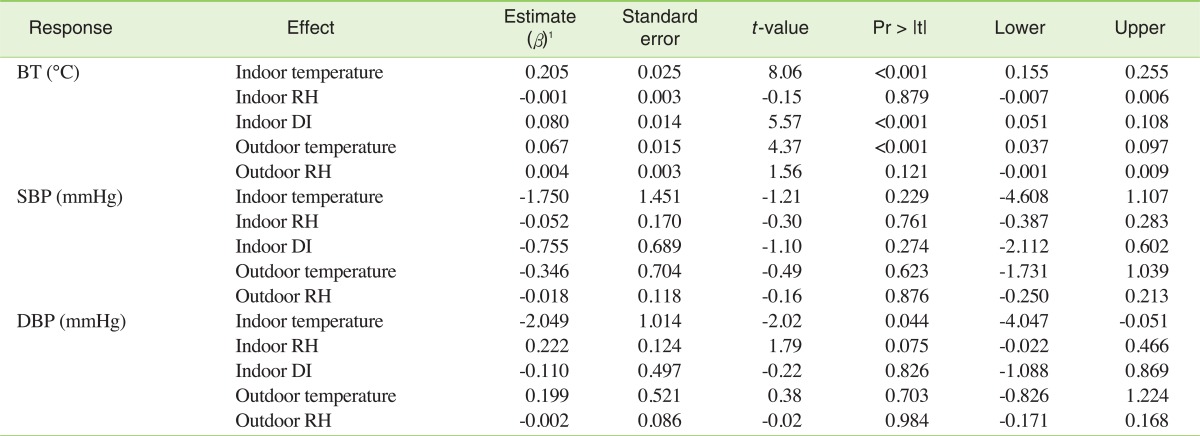 BT, body temperature; RH, relative humidity; DI, discomfort index; SBP, systolic blood pressure; DBP, diastolic blood pressure 1All effects of climatic variables were results from multivariate models. In the model for body temperature, sex and age were included, and in case of blood pressure, sex, age, current smoking habit, alcohol consumption, and measurement time (morning and afternoon) were included for adjustment. Table 4Comparison of the effects of indoor temperature and relative humidity between hypertension and non-hypertension elderly group  BT, body temperature; RH, relative humidity; SBP, systolic blood pressure; DBP, diastolic blood pressure. 1All effects of climatic variables were results from multivariate models. In the model for body temperature, sex and age were included, and in case of blood pressure, sex, age, current smoking habit, alcohol consumption and measurement time (morning and afternoon) were included for adjustment. |
|
|||||||||||||||||||||||||||||||||||||||